Millions of people around the world are following a priority to have a healthy heart. Blockage in heart arteries is one of the most common risks that pose a grave condition in the form of heart attack or stroke. Medical treatment is necessary when a coronary artery is blocked, and the artery needs to be opened up once again so that further complications may not occur. Placing stents might be the best treatment ever.
This post has a quick guide to the essentials: how stents work, who needs them, and what you should expect beforehand and after the process.
What Are Heart Arteries and Why Do They Get Blocked?
The coronary arteries provide oxygen-rich blood to the heart. High cholesterol, high blood pressure, smoking, and a poor diet can all increase deposits of atherosclerosis or plaque in the arteries over the course of years, narrowing them. A blockage in the heart is caused by this limitation of blood flow, which can be accompanied by symptoms such as chest pain or angina, shortness of breath, and others.
Blockage in the heart is mostly associated with the disease known as atherosclerosis, which involves plaque that continues to accumulate, thereby narrowing the arteries progressively. This may go up to the complete blocking of the blood vessels. It can cause a heart attack due to the lack of oxygen reaching the heart muscles if it is not attended properly.
There could be underlying symptoms that occur before this blockage in the heart, such as chest pain or discomfort, fatigue, and dizziness. Generally, these warning signs might call for medical professionals to evaluate them and, upon finding the need for dilation of the obstructed artery to ensure the free flow of blood, use medical devices like stents.
What are Stents and How Do They Work?
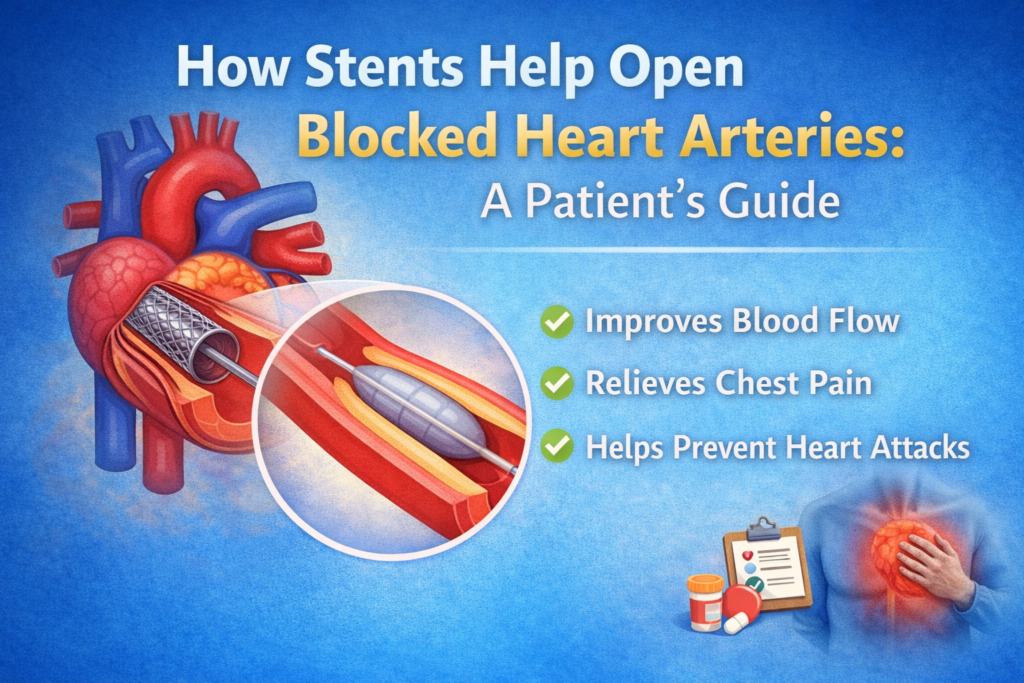
So, what are stents? Simply put, a stent is a small, expandable tube introduced into a blocked artery to keep the artery open. It will restore flow through narrowed and obstructed arteries by breaking up plaque. Most commonly, stents are made of metal, but sometimes they may be coated with medicines that help prevent more plaque from accumulating in the treated area. Such stents are referred to as drug-eluting stents.
This scaffolding supports the walls of the arteries such that they do not collapse or narrow again once the blockade is cleared. The procedure is called angioplasty, whereby a balloon-tipped catheter is inserted within the narrowed artery, which is inflated to widen the artery, and the stent gets deployed to hold the artery open in case the balloon is deflated and removed.
Bare-metal stents and drug-eluting stents represent two extremes of options available. Bare-metal stents are uncoated and operate physically to prevent re-narrowing in the artery. Drug-eluting stents are coated with medication and delivered slowly over time so that there is less chance of scar tissue forming around the stent, lower chances for the blockage in the heart.
The process is referred to as percutaneous coronary intervention, or PCI, but is more widely known as an angioplasty. It can be carried out on an awake patient who is sedated. Here’s what happens:
- Preparation: The doctor will start by introducing a catheter into the blood vessel, preferably in the wrist or groin and advance it up to the coronary arteries. This is done using a form of X-ray known as fluoroscopy.
- Dilatation by Balloon Inflation: Once the catheter reaches the area where there is a blockage at the heart end, the tip of the catheter with a very small balloon will be inflated. This will bulge the plague against the walls of the artery and hence it will dilate it.
- Placement of Stent: A stent is placed on the balloon. When the balloon expands, the stent expands and remains in place; the artery is ensured to be open even as the balloon deflates and is withdrawn.
- Follow-Up Post Procedure: The stent remains inside permanently, and blood can flow through the artery, undeterred. A patient leaves the hospital the following day. Recovery takes a few weeks.
The main benefits of this process include preventing the heart from ever becoming fully obstructed, which can potentially lead to a heart attack. As the stent will remain inside the artery for life, follow-up care and lifestyle changes will be important to maintaining long-term effectiveness.
Who Needs a Heart Stent?
Not all patients suffering from blockage in heart require a stent. Additional factors are taken into consideration by physicians to recommend this treatment. A stent is usually prescribed in patients whose coronary arteries have wide-scale narrowing or obstruction, thereby reversing the blood flow and preventing further complications.
A stent is usually recommended for patients who suffer severe angina or chest pain because of decreased blood flowing to the heart.
- People who have had a history of heart attack where the blockage has left the part of the heart muscle de-oxygenated and cut off from its blood supply
- All coronary artery patients, particularly in situations when medicine and adjustments in lifestyle cannot control the condition properly
Doctors may perform a test called an angiogram to determine the severity of obstruction in the heart before placing a stent. The angiogram will depict an extensive view of blood vessels, which can help a doctor measure the degree of narrowing or obstruction.
Benefits of Stents in Treating Blocked Arteries
The overall goal of stenting is to restore normal blood flow through the heart’s arteries. It enhances the potential candidate’s quality of life and decreases the likelihood of heart attack by decreasing signs and symptoms like chest ache and weariness.
Some of the main benefits include:
- Flow in the blood: Stents hold an artery open so that oxygen-rich blood may continue to flow freely to the heart muscle with reduced heart strain.
Lower Risk of Heart Attack: A stent guarantees the complete opening of the heart, which directly reduces the risk of having a heart attack.- Relief of Symptoms: Most patients can be allowed to spend a considerable amount of time after angioplasty with a stent without the symptoms such as chest pain and shortness of breath that are associated with blockage in the heart.
- Speedy Recovery: Angioplasty with a stent is minimally invasive, meaning the patient recovers faster than when undergoing open-heart surgery.
Though the procedure is highly effective, patients need to be heart-healthy after surgery in order to avoid future complications.
Risks and Complications with Stent Placement
Like any medical procedure, there are always risks involved, but they are very low. Patients often recover quite smoothly with few complications. The possible complications include:
- Blood Clots: Blood clots may sometimes occur inside the stent post-implantation. The chance of heart attack is high, so blood thinners are given by physicians.
- Re-narrowing of Arteries: Scar tissues may develop around the stent in some instances that go on to cause narrowing of the artery again. That’s another factor with bare metal stents not as popular; drug-eluting stents can be used more.
- Bleeding or Infection: Similar to any other catheter insertion procedure, there is a small risk of bleeding or infection at the insertion site.
Discussing these risks with your doctor will be helpful so you’ll have an idea of the possible complications and how they can be managed for a better outcome.
Life After Stent Placement: Medications and Lifestyle Changes
After the installation of stents, life does not become centered around a new normal. There are several things that the patients should observe themselves if they wish to succeed in the long term.
- Medications: Blood-thinning medications, like aspirin or clopidogrel, are prescribed to avoid blood clots from forming around the stent. Such medications are typically taken for one year or more contingent on the kind of stent installed.
- Diet and exercise: Dietary intervention includes a heart-healthy diet, which consists of fruits, vegetables, whole grains, and lean proteins. Regular physical activity, whether it is walking, swimming, or cycling, also affects the keeping of the heart healthy.
- Follow-Up Care: The cardiologist is consulted periodically to monitor whether the stent keeps the artery fully open or not and an early sign of the narrowing back-up or some other complications.
The lifestyle modification is very essential to prevent future blocking of the heart. A smoker should quit smoking, while those who have cholesterol or high blood pressure must work hand in hand with their healthcare provider to manipulate these conditions.
Conclusion
Heart stenting is an effective treatment for patients who are diagnosed with coronary artery disease or with a block in their heart. Stents help to open the arteries thereby allowing the blood to pass through those pathways again and drastically lessening the opportunity for a heart attack. This will greatly improve the quality of life for a patient.
In itself, the procedure is rather straightforward. However, long-term success requires a good lifestyle, adherence to prescribed medications, and an eye that is open to cardiac health. If you find yourself in a position of having stent placement, it is helpful to know how the procedure is done and what benefits there can be so you can make informed decisions regarding your heart’s health.